CZMD
ACL Tears and Treatment
Patient Testimonial: "Dr. Ziegler performed ACL construction w/ patellar tendon graft and scoped meniscus in April 2019. As an endurance runner and avid skier, I was apprehensive of recovery and strength. 8 months from surgery, and I am feeling great and knee is strong. Long road to recovery but with his guidance and recommendations along with protocol for rehab, I'm way ahead of schedule with recovery. Very pleased with outcome and highly recommend Connor and his team at NEOS!!" ~ JW
Definition of ACL tear:
The anterior cruciate ligament (ACL) is the most important ligament of the knee to prevent the knee from sliding forward or rotating anterolaterally. Patients who sustain an ACL tear often have problems with twisting and turning activities, such as in playing football, soccer, or skiing, and will often require an ACL reconstruction to provide stability to their knee.
In addition to its stability role in the knee, the ACL also protects the menisci (shock absorbers) of the knee. When the knee continues to have instability events after an ACL tear, it is not uncommon to have either the medial or lateral meniscus tear. ACL reconstructions are performed in patients who note instability and/or participate in twisting, turning, and pivoting sports to ensure that they do not tear their menisci and develop osteoarthritis later in life. The patient’s age, activity level and grade of tear will determine the correct treatment option.
An ACL tear is classified by the amount of injury to the ligament:
• Grade I: a partial ACL tear
• Grade II: near complete ACL tear
• Grade III: a complete ACL tear – the ligament is non-functional.
Description of ACL Reconstruction
An ACL surgery requires precise knowledge of the anatomy of the knee, attachment sites of the ACL and knowledge on the other ligaments and structures of the knee. When not replacing the ACL at its correct attachment sites or if other concurrent injuries are not treated, there is a much higher risk of ACL graft failure. On the tibia (shinbone), the tunnels should be in line with the posterior margin of the anterior horn of the lateral meniscus. On the femur (thigh bone), the reconstruction tunnel should be placed at the midpoint of the attachment bundles (anteromedial and posterolateral bundles of ACL), with the main portion of the reconstruction tunnel being posterior to the lateral intercondylar ridge.
ACL anatomy and landmarks on the tibia (left) and femur (right) from 2011 article published by Dr. Ziegler and co-authors.
Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. The American journal of sports medicine. 2011 Apr;39(4):743-52.
In general, a well-done ACL reconstruction can function quite well for 20 years or longer based on the data we have in scientific studies on ACL reconstruction grafts. The main risk for ACL reconstructions failing long term is in those patients who had their meniscus taken out rather than repaired. These patients are at a much higher risk for the development of osteoarthritis.
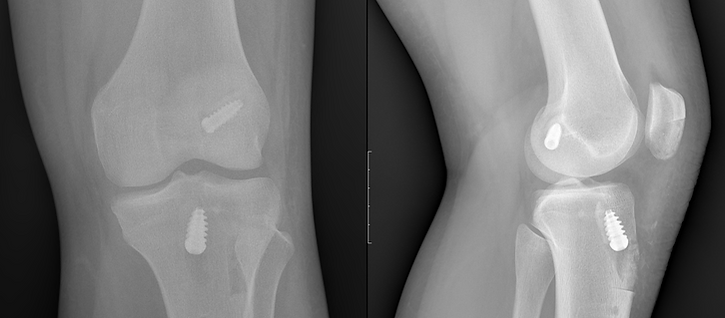
Dr. Ziegler’s anatomic ACL reconstruction technique involves using a patellar tendon autograft (from the patient’s own tissues). It is called a “BTB” graft because it takes bone off the patella, uses a strip of patella tendon, and then takes a piece of bone off the tibia. A reconstruction tunnel is drilled at the anatomic attachment sites of the ACL on the tibia and femur. The patellar tendon graft is pulled into the joint and fixed in place with titanium interference screws. The use of the autograft allows the patient to return to activities sooner with less risk of reconstruction graft failure. Other graft options including soft tissue autograft (hamstring or quadricep tendon) or allograft may be used in special circumstances and discussed pre-operatively. If there are any associated repairable meniscus tears, it is also recommended to repair these tears to both protect the ACL grafts and minimize the risk of arthritis over time.
Post-surgery X-rays on a high level soccer player after ACL reconstruction performed by Dr. Ziegler using BTB autograft and titanium screw fixation.
Post-Operative Protocol for ACL Reconstruction
It is absolutely essential for a physical therapist to be consulted following ACL surgery. Reactivation of the quadriceps mechanism, edema control, patella mobilization, maintenance of full knee extension and regaining knee motion are absolutely essential to obtaining optimal post-operative outcomes. Dr. Ziegler has a specific protocol that his patients are provided to guide their therapy and recovery.
Frequently Asked Questions
What is ACL reconstruction surgery and how is it done?
ACL reconstruction surgery consists of replacing a torn ACL with another ligament or tendon. This can be from one’s own body (an autograft) or from a donor (an allograft). In an ACL surgery, tunnels are reamed at the normal attachment site of the ACL on both the femur and tibia, and the graft is secured either inside or outside these tunnels. There are multiple ways to secure the graft, and this can include fixation within the tunnels with metal or bioabsorbable/plastic screws or through a loop and button placed on the outside of the tunnels. In general, the fixation of the grafts is performed according to the way the surgeon was trained, with the gold standard being screws placed within the tunnels for patellar tendon grafts and looped sutures with cortical buttons or screws within tunnels for hamstring ACL reconstruction grafts. The type of graft to use (autograft vs allograft) can depend on multiple factors. This can include the patient’s age, whether or not they have hyperlaxity, what type of sports they play, and other factors.
When should ACL surgery be performed?
Athletes who have any difficulty with twisting, turning, or pivoting after an ACL tear should consider having their ACL reconstructed. This is because repeated twisting and turning mechanisms can damage both the cartilage and the menisci (shock absorbers) of the knee. The medial meniscus is the most at risk to injury with an ACL tear because it compensates for the torn ACL when to prevent the knee from slipping forward. In addition, patients who may have a repairable meniscus tear at the time of their ACL tear should consider surgery to prevent the tear from becoming non-reparable. In general, most people who tear their menisci develop arthritis and symptoms within 8-10 years after their ACL tear. Thus, one of the main reasons for the general public to consider having an ACL reconstruction is to treat any repairable meniscus tears, and also to prevent meniscal tears from developing later in an unstable knee.
When should an ACL be repaired rather than reconstructed?
ACLs can be repaired is when an ACL is torn with a piece of bone, usually off the tibia, which is much more common than when torn off the femur. There are perhaps 10% of patients who may have injury only to the attachment site on the tibia or femur and do not have ACL intrasubstance stretch or tear. These injuries must be treated in the “acute” situation, which can vary anywhere from days to just a few weeks. In these cases, the bony piece can be fixed at the normal attachment site with sutures or a screw and early motion can begin. In those instances where the tissue is not strong enough to allow early motion, there is a much higher risk of stiffness if immobilization is required after surgery. Research is still ongoing to try to improve outcomes because attempts at repairs in the literature previously have not shown good outcomes over time. To date, the outcomes presented at scientific meetings is quite variable with a failure rate of anywhere from 20% to 80%. Therefore, one should be cautious about considering an ACL repair over reconstruction. More research is necessary to define better techniques to perform ACL repairs, and it is important that these techniques be based upon good science and not on marketing by device companies because previous attempts at ACL repairs did not show failures until after two years after surgery.
How long does it take an ACL reconstruction to heal?
The healing process for an ACL reconstruction graft can depend upon the type of graft. In general, patellar tendon grafts heal into the bone tunnels at 6 weeks. Hamstring tendon grafts may take up to 3 months to heal in the tunnels, whereas cadaver grafts can take 3 months or longer. In terms of the main graft substance healing that is within the joint, it is generally at its weakest point between 3 and 4 months after surgery, and having a good blood supply restored to the tissue can take 9 to 12 months or longer.
What type of ACL reconstruction should be performed for a teenager?
The International Olympic Committee statement reports that teenagers who tear their ACL should have an ACL reconstruction sooner rather than later to protect against cartilage damage and meniscus tears, which can lead to development of osteoarthritis (loss of cartilage). One of the most important things to assess in the teenager is if their growth plates remain open or not. If the growth plates are still open, then placement of bone plugs or fixation hardware across the growth plates should be avoided to minimize the risk of a growth plate arrest. Usually, this means that these patients have ACL reconstructions with hamstring grafts or quadricep tendon graft. ACL reconstructions in teenagers is very problematic because multiple studies have reported that the risk of an ACL tear in either the same knee or the opposite knee is roughly 30%. It is especially important in teenagers to ensure that they have a full return of strength, endurance, agility, and balance prior to returning back to sports because their risk of re-tear can be much higher if they do not pass some type of functional sports assessment.
When can an ACL reconstruction be performed in those over age 60?
There is no upper age limit to an ACL reconstruction because it is mainly dependent upon the patient’s activity levels, other medical problems and whether they have instability. For older patients with ACL tears, we commonly place them into an ACL brace to see if that will be sufficient to restore their stability and function. If one has continued instability, swelling and functional limitation despite bracing without significant underlying arthritis, it may be indicated to proceed with an ACL reconstruction. If the patient has significant underlying arthritis in addition to an ACL tear, a knee replacement is a more durable option for both relief of pain and instability.
How long is the recovery after ACL surgery?
One of the most important things for preventing ACL reconstruction failure is to regain strength of the thigh muscles. In the past, many surgeons tried to get their patients back to full activities by 5 or 6 months, which resulted in higher failure rates. More recent data has suggested that waiting up to 12 months or more until return to sports (especially in young athletes) may be better because the retear goes down significantly. In general, it is important to make sure that an athlete has fully regained proprioception, strength, agility, and endurance to minimize their risk of reinjury.
When I can run after ACL surgery?
Several factors are involved in determining return to running. If an ACL reconstruction was performed without additional surgery, there are no other ligaments or meniscus injuries, the cartilage surfaces are intact, and a proper rehabilitation program was completed; then starting a gradual return to running program can begin around 4-5 months post-op. Having appropriate quadriceps strength is the main factor prior to starting to run again. In general, an athlete should wait a minimum of 4 months after their ACL reconstruction to return to running on even surfaces. We have the patient perform a single-leg squat with no bending of the knee inwards (valgus collapse) during the single leg squat. If the patient has a good return of function, good motion, and does not have a valgus collapse when performing a single-leg squat; they are generally able to initiate a return to running program. This allows the quadriceps mechanism to be strong enough to prevent extra stress on the knee, which can lead to knee swelling and further injury.
When can I golf after an ACL reconstruction?
It is important to have good restoration of strength and stability prior to returning back to golfing. In most circumstances, with a first-time ACL reconstruction and no other significant injuries to the knee, return to golf can begin around 4 months after surgery.
When can I go back to work after an ACL reconstruction?
Returning back to work after an ACL reconstruction is a very individualized decision. In those people who have desk jobs, they can often return back to work for partial work days within 7 to 10 days, as long as they can ice and elevate their knee to minimize swelling. For those patients who require the use of ladders, stairs, twisting, turning, or lifting; the time can vary from 3 to 6 months after surgery, depending upon the type of graft, associated other surgeries with the ACL reconstruction, and status of overall strength and endurance.
What causes ACL reconstruction to fail?
The primary reason of ACL reconstruction failure in the literature is improperly placed ACL grafts at the initial surgery. This can cause extra stress on an ACL reconstruction graft, which can lead to its failure. A large number of ACL reconstruction graft failures are in those patients who have the graft placed too posterior (central) on the tibia, too anterior on the femur, or too central on the femur (effectively only reconstructing the anteromedial bundle). These locations can lead to stretching of the reconstruction graft or failure to control knee rotational laxity.
One of the highest risk factors for an ACL graft failure is a patient who has a cadaver graft, called an allograft, when they are 25 years or less of age. The failure rate for these can be up to 40% or more in some series. In addition, other ligament injury missed at the time of the ACL surgery, such as an MCL or a posterolateral corner injury, can also put significant stress on an ACL reconstruction graft, which can lead to its failure. Other factors that can cause an ALC graft to fail can include tears of the posterior horn of the medial meniscus. This is because the posterior horn of the medial meniscus is a secondary restraint preventing the knee from sliding forward. In patients who may not have their medial meniscus, the ACL graft generally tends to be looser than in patients who do have their medial meniscus. Thus, in some patients, this can lead to the graft being overloaded and it can cause the ACL graft stretch out over time.
Other factors that can lead to ACL reconstruction failure are patients that have soft tissue grafts, such as hamstrings grafts, that have hyperlaxity. Patients who have a lot of knee hyperextension or significant increase of heel height (more than 4-5 cm) have a much higher risk of their ACL graft stretching out versus a patellar tendon graft. Other factors include patients with a large increase in their posterior tibial slope (sagittal plane tibial slope), which can cause an ACL graft to be overloaded and stretch out over time.
Patellar tendon versus hamstrings versus quadricep tendon ACL reconstruction:
Patellar tendon ACL reconstructions have been considered the gold standard for decades. This is because they are the graft of choice for physicians who cover high level athletes; however, hamstrings grafts are also appropriate for a large number of patients. Hamstrings grafts are appropriate for patients with open growth plates and in those patients who may have lower levels of activity desired after an ACL reconstruction. In general, a patellar tendon ACL reconstruction should not be performed in patients with significant arthritis of their kneecap joint, or those who have had previous patellar tendon harvest or patellar tendon repair. Hamstring ACL reconstruction grafts should definitely not be considered in patients with significant hyperlaxity, such as in patients with a large heel height, because these grafts have been shown to stretch out over time. In general, the large data base series have reported that the retear rate is lower with a patellar tendon reconstruction compared to a hamstrings ACL reconstruction. However, a well done ACL reconstruction with either graft can be appropriate for the majority of patients.
The use of a quadriceps tendon autograft for ACL reconstructions is a newer graft choice for many people. It is felt to possibly be a better option for some pediatric patients then utilizing the hamstring grafts because the graft volume may be larger. In terms of adults, there is not enough good science presently to decide whether the graft should be used with a bone plug or not, if there should be a full-thickness or partial-thickness graft, and if the rehabilitation protocols should be changed. To date, BTB (patella tendon) graft still has the best data to support its use with lowest failure rate among graft options.